Claims Management
Decision making tool for pre-authorisation that enables automated coverage and completeness checks, and advanced quote analysis thanks to medical coding coherence and pricing benchmarks.
What we offer
- Automated extraction of relevant information and using trained AI to determine relevant coverage check details from underlying term/conditions and policies database
- Automated decision based on matching the provided claims information and the trained conditions
- Quote analysis using benchmarking & pricing analysis and medical coding coherence checks
- Qantev patient journey analysis to check if service is necessary & suitable
- Alternative provider recommendation for SMO
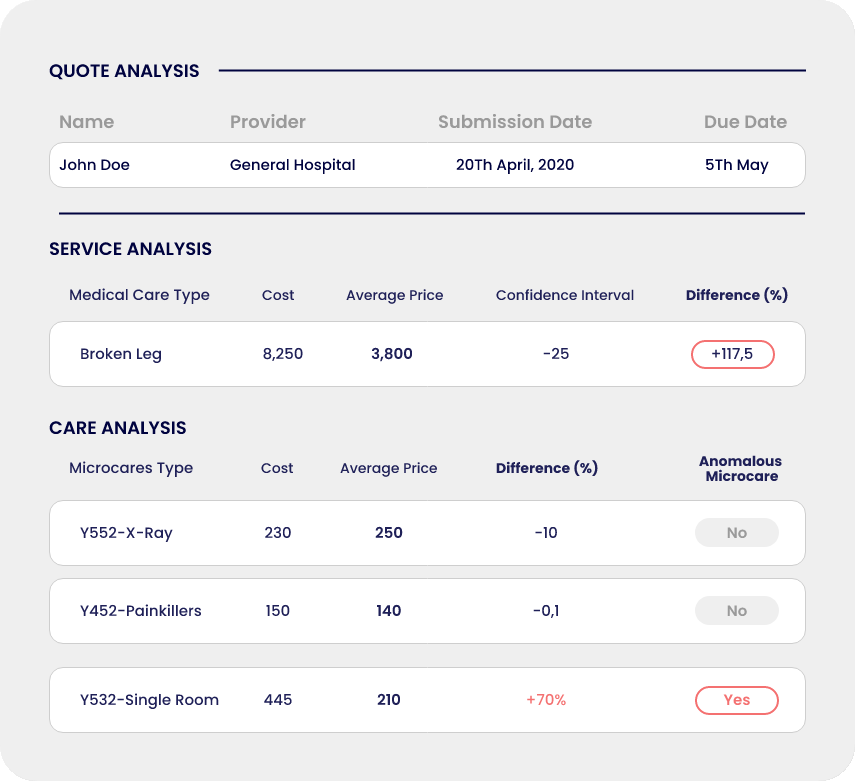
QUOTE ANALYSIS
Pre-authorisation analysis report
Qantev provides comprehensive quote analysis using pricing benchmark and medical coding coherence checks. Claims manager also gets insights about patient journey.
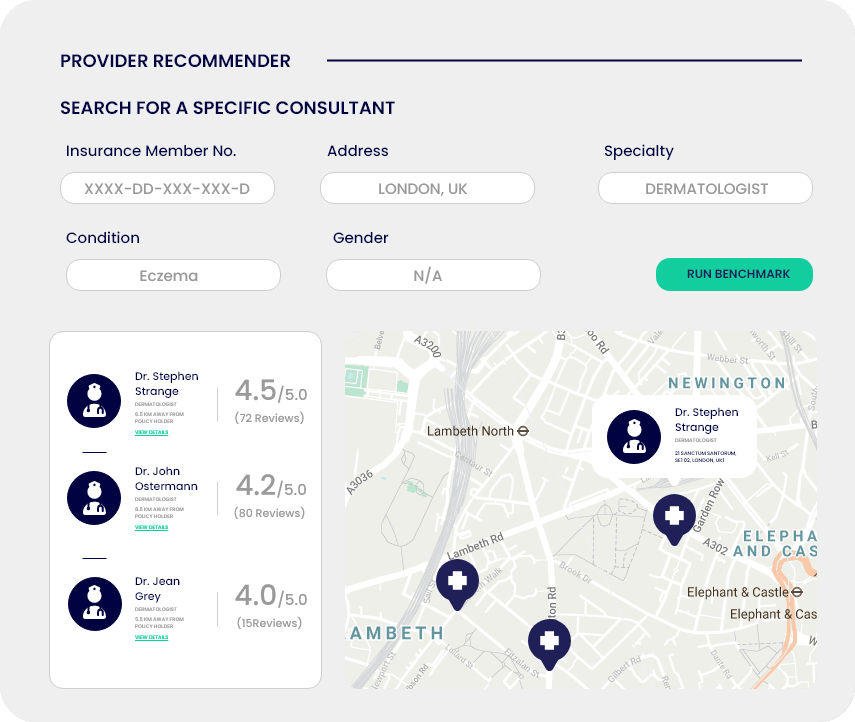
PROVIDER RECOMMENDER
Alternative provider recommendation
Using historical claims, patient profile and multiple data points, Qantev can help identify the best alternative provider for referrals or second medical opinions.
NORMALISED QUOTE TABLE
PROVIDER SERVICE QUALITY
ALTERNATIVE PROVIDER RECOMMENDATION
How We Do It
Qantev’s multiple highly specialised technological assets are enabling straight through processing capabilities thanks to automated coverage and completeness checks, while improving customer experience with quicker communication.
NEXT